In the realm of medical conditions, stress ulcers stand out as a prevalent and potentially severe issue that affects the lining of the stomach and sometimes the duodenum, the initial segment of the small intestine. These ulcers, often referred to as acute gastric ulcers, are characterized by erosions that extend into the mucosa, the innermost layer of the stomach lining. This article delves into the intricacies of stress ulcers, encompassing their causes, manifestations, and the multifaceted strategies employed in their management.
The genesis of stress ulcers can be attributed to numerous factors, encompassing severe stress, trauma, major surgical interventions, burns, sepsis, and even certain medications like nonsteroidal anti-inflammatory drugs (NSAIDs). These stressors inflict a cascade of physiological responses, including an elevation in gastric acid secretion, a disruption of the stomach’s mucosal barrier, and a reduction in blood flow to the stomach lining. This perfect storm of events sets the stage for the formation of stress ulcers, which can range in size from a few millimeters to several centimeters.
Unveiling the Signs and Symptoms of Stress Ulcers and Navigating the Management Maze
What is a Stress Ulcer and How is it Managed
Understanding stress ulcers and their management.
- Stressors: Trauma, burns, surgery.
- Pathophysiology: Acid, ischemia, barrier disruption.
- Clinical Presentation: Abdominal pain, bleeding.
- Diagnosis: Endoscopy, biopsy.
- Management: Proton pump inhibitors, mucosal protectants.
- Prevention: Stress reduction, prophylactic medications.
- Complications: Bleeding, perforation.
Stress ulcers require prompt diagnosis and management to prevent complications.
Stressors: Trauma, Burns, Surgery
Stress ulcers are often triggered by severe stressors that place immense physiological strain on the body. These stressors can be broadly categorized into three groups: trauma, burns, and surgery.
Trauma
Traumatic injuries, such as those sustained in motor vehicle accidents or falls from a height, can lead to the development of stress ulcers. The body’s response to trauma involves a cascade of hormonal and inflammatory changes that can disrupt the normal protective mechanisms of the stomach lining, making it more susceptible to ulcer formation.
Burns
Extensive burns, particularly those involving more than 20% of the body surface area, are another major stressor that can precipitate stress ulcers. The inflammatory response to burns releases a surge of hormones and inflammatory mediators that can impair the stomach’s mucosal barrier, increasing the risk of ulceration.
Surgery
Major surgical procedures, especially those involving the abdomen, can also contribute to the development of stress ulcers. The surgical trauma, coupled with the use of anesthesia and opioids, can disrupt the normal physiological functions of the stomach, leading to an increased susceptibility to ulcer formation.
These stressors share a common pathway of inducing a hyperinflammatory state, which disrupts the delicate balance of the stomach’s mucosal lining. This disruption allows gastric acid and other harmful substances to penetrate the mucosa, causing erosion and ulceration.
Pathophysiology: Acid, Ischemia, Barrier Disruption
The development of stress ulcers is a complex process involving a trifecta of factors: increased gastric acid secretion, impaired mucosal barrier function, and reduced blood flow to the stomach lining.
- Increased Gastric Acid Secretion:
Stressful conditions trigger the release of hormones and inflammatory mediators that stimulate the production of gastric acid. This excess acid overwhelms the stomach’s natural defenses, creating an acidic environment that can erode the mucosal lining and promote ulcer formation.
- Impaired Mucosal Barrier Function:
The stomach lining is protected by a mucosal barrier that acts as a shield against gastric acid and other harmful substances. Stressors can disrupt the integrity of this barrier by damaging the cells that produce protective mucus and bicarbonate, making the mucosa more vulnerable to erosion and ulceration.
- Reduced Blood Flow:
Stress can also lead to a reduction in blood flow to the stomach lining. This impaired blood supply deprives the gastric mucosa of oxygen and nutrients, further compromising its ability to resist the damaging effects of gastric acid and other injurious factors.
The combination of these three factors—increased acid secretion, impaired mucosal barrier function, and reduced blood flow—creates a perfect storm that sets the stage for the development of stress ulcers.
Clinical Presentation: Abdominal Pain, Bleeding
Stress ulcers often manifest with a constellation of symptoms, the most common of which are abdominal pain and bleeding.
- Abdominal Pain:
The pain associated with stress ulcers is typically located in the upper abdomen, just below the rib cage. It may be described as a burning, gnawing, or aching sensation that worsens with eating or drinking. The pain may also be accompanied by nausea, vomiting, and bloating.
- Bleeding:
Stress ulcers can cause bleeding, which may range from minor to severe. Patients may experience hematemesis (vomiting of blood) or melena (black, tarry stools). In some cases, the bleeding may be so severe that it leads to anemia and shock.
It’s important to note that stress ulcers can also be asymptomatic, meaning they may not cause any noticeable symptoms. This is why early diagnosis and management are crucial to prevent complications.
Diagnosis: Endoscopy, Biopsy
Confirming a diagnosis of stress ulcers typically involves a combination of endoscopic examination and biopsy.
- Endoscopy:
Endoscopy is a minimally invasive procedure that allows the doctor to directly visualize the lining of the stomach and duodenum. During an endoscopy, a thin, flexible tube with a camera attached is inserted through the mouth and into the digestive tract. The doctor can then carefully examine the mucosal lining for any signs of ulcers, erosion, or bleeding.
- Biopsy:
If suspicious lesions are identified during endoscopy, the doctor may perform a biopsy. This involves taking a small sample of tissue from the ulcerated area using a biopsy forceps. The tissue sample is then sent to a laboratory for analysis, which can confirm the presence of stress ulcers and rule out other conditions with similar symptoms.
In some cases, additional tests may be necessary to assess the severity of the stress ulcers and to rule out other potential causes of the symptoms, such as blood tests or imaging studies.
Management: Proton Pump Inhibitors, Mucosal Protectants
The cornerstone of stress ulcer management revolves around two mainstays: proton pump inhibitors (PPIs) and mucosal protectants.
Proton Pump Inhibitors (PPIs):
PPIs are a class of medications that potently suppress gastric acid secretion. By reducing the acidity of the stomach contents, PPIs create a more favorable environment for ulcer healing and help prevent further erosion of the mucosal lining. PPIs are typically administered intravenously in critically ill patients or orally in those who are able to tolerate oral medications.
Mucosal Protectants:
Mucosal protectants are agents that help protect the stomach lining from further damage and promote healing. There are several types of mucosal protectants, including:
- Sucralfate: Forms a protective barrier over the ulcer, shielding it from gastric acid and pepsin.
- Misoprostol: A synthetic prostaglandin analog that helps maintain the integrity of the mucosal lining and reduces gastric acid secretion.
- Antacids: Neutralize stomach acid, providing quick relief from pain and discomfort.
The choice of specific medications and the duration of treatment will depend on the severity of the stress ulcers, the underlying cause, and the patient’s individual needs and response to therapy.
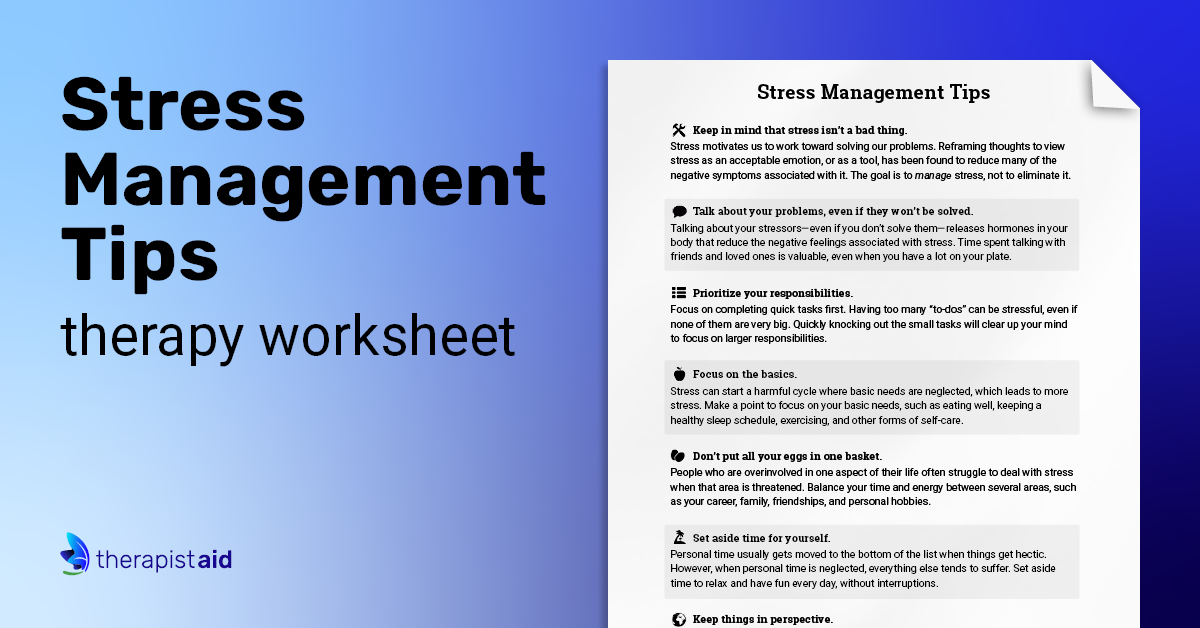
Prevention: Stress Reduction, Prophylactic Medications
Preventing stress ulcers involves a multifaceted approach that encompasses stress reduction techniques and the judicious use of prophylactic medications.
- Stress Reduction:
Minimizing stress, especially in high-risk situations, can significantly reduce the likelihood of developing stress ulcers. This may involve employing relaxation techniques, such as deep breathing exercises, meditation, or yoga, to manage stress levels.
- Prophylactic Medications:
In certain high-risk scenarios, prophylactic medications may be prescribed to prevent stress ulcers. These medications typically include:
- Proton pump inhibitors (PPIs): Suppress gastric acid secretion.
- Histamine-2 receptor antagonists (H2RAs): Reduce gastric acid production.
- Sucralfate: Forms a protective barrier over the stomach lining.
The decision to use prophylactic medications is typically made on a case-by-case basis, taking into account the patient’s risk factors, overall health status, and potential benefits and risks of the medications.
Complications: Bleeding, Perforation
While stress ulcers are often manageable with proper treatment, they can potentially lead to serious complications if left untreated or inadequately managed.
- Bleeding:
Stress ulcers can cause significant bleeding, which may manifest as hematemesis (vomiting of blood) or melena (black, tarry stools). Severe bleeding can lead to anemia, shock, and even death if not promptly addressed.
- Perforation:
In severe cases, stress ulcers can erode through the entire thickness of the stomach or duodenal wall, leading to perforation. This is a life-threatening condition that can cause peritonitis, a serious infection of the abdominal cavity. Perforation requires immediate surgical intervention to repair the perforation and prevent life-threatening complications.
Early diagnosis and proper management of stress ulcers are crucial to prevent these complications and ensure a favorable outcome.
FAQ – Stress Management
To shed more light on stress management’s significance, let’s address some commonly asked questions.
Question 1: Why is stress management important?
Stress management is vital because chronic stress can significantly impact our physical and mental well-being.
Question 2: What are some common signs of stress?
Stress often manifests through physical symptoms like headaches, muscle tension, and digestive issues. It can also lead to emotional and behavioral changes, such as irritability, anxiety, and difficulty concentrating.
Question 3: How can I manage stress effectively?
Effective stress management techniques include exercise, relaxation methods (deep breathing, meditation, yoga), maintaining a balanced diet, getting enough sleep, and seeking support from friends, family, or professionals.
Question 4: What are some lifestyle changes that can reduce stress?
Adopting a healthy lifestyle, including regular physical activity, a balanced diet, sufficient sleep, and avoiding excessive caffeine and alcohol consumption, can significantly reduce stress levels.
Question 5: When should I seek professional help for stress management?
If stress becomes overwhelming and starts interfering with daily life, relationships, or overall well-being, seeking professional help from a therapist or counselor is recommended.
Question 6: How can I incorporate stress management into my daily routine?
Simple strategies like taking short breaks, practicing mindfulness, engaging in hobbies, and spending time in nature can be easily incorporated into daily life to manage stress.
Remember, stress management is an ongoing process that requires self-awareness, practice, and seeking support when needed. Prioritizing well-being and implementing effective stress management techniques can lead to a healthier and more balanced life.
For further guidance, here are some additional tips to help alleviate stress.
Tips for Stress Management
Incorporating stress management techniques into daily life can significantly improve well-being. Here are four practical tips to help you get started:
Tip 1: Practice Relaxation Techniques:
Engage in activities that promote relaxation and reduce tension. Deep breathing exercises, meditation, yoga, and progressive muscle relaxation are effective techniques for calming the mind and body.
Tip 2: Maintain a Balanced Lifestyle:
Prioritize a healthy diet, regular physical activity, and adequate sleep. These elements contribute to overall well-being and resilience to stress.
Tip 3: Nurture Meaningful Relationships:
Spend time with loved ones, engage in social activities, and seek support from friends and family. Strong social connections can provide a buffer against stress.
Tip 4: Seek Professional Help if Needed:
If stress becomes overwhelming or negatively impacts daily life, seeking guidance from a therapist or counselor can be beneficial. They can provide personalized strategies and support to manage stress effectively.
Remember, stress management is an ongoing process. Implementing these tips and adapting them to your unique needs can lead to a healthier and more balanced life.
By prioritizing self-care, practicing stress management techniques, and seeking support when needed, you can take control of your stress and improve your overall well-being.
Conclusion
Stress is an inevitable part of life, but how we manage it can significantly impact our physical and mental well-being. This article delved into the intricacies of stress ulcers, their causes, manifestations, and management strategies, emphasizing the importance of stress reduction and prophylactic measures. Additionally, we explored stress management techniques and provided practical tips to help individuals cope with stress effectively.
The key to successful stress management lies in recognizing the impact of stress on our lives and taking proactive steps to reduce its negative effects. Whether it’s implementing relaxation techniques, maintaining a balanced lifestyle, seeking support from loved ones, or seeking professional help when needed, prioritizing self-care and well-being is essential.
Remember, stress management is a journey, not a destination. It requires ongoing effort, self-awareness, and a willingness to adapt strategies to unique needs and circumstances. By embracing stress management as a lifelong practice, we can cultivate resilience, enhance our overall health, and lead more fulfilling lives.
Images References :

Woody Beck, a happy parents with two kids.